This current revision of the criteria is actually quite similar to the original release. The criteria are now reorganized into five buckets. Those buckets, or groupings, of the new criteria are as follows:
- Inclusive Teaching and Learning
- Addressing Public Health Priorities
- Creating Behavioral Change
- Demonstrating Leadership
- Achieving Outcomes
It should be noted that at this time these criteria are not applicable to CE providers accredited under the aegis of the Joint Accreditation Task Force.
Menu of Choices
Importantly, the long-promised menu of choices has finally been revealed. This means that providers that wish to demonstrate the advanced commendation criteria will now have a choice as to which of the 15 new criteria they implement. Thus, providers will choose from among the 15 advanced criteria from those that fit naturally within the environment of their unique organization. Providers must select eight of the 15 criteria, and among those eight at least one must be from each of the five buckets listed above. The remaining three choices may come from any of the groupings.
Transition Period
Once the final publication of the new criteria is released in the summer of 2016, the ACCME will allow an adequate transition period—probably one year—in which providers will begin to implement them and transition from the old “Engagement” criteria to the new criteria. Providers whose self-studies occur during that transition will have the choice of keeping the old criteria or move to the new criteria, but not a mix of the two.
More Specificity and a Standard for Compliance
With the release of these new criteria, the ACCME has provided better definitions and interpretation of each criterion and an outline of the standard by which a provider can determine what will constitute compliance. These criteria will be judged to be in compliance based on two factors:
1. Frequency, as defined by the percent of activities that must demonstrate compliance
2. Substantive manifestation of the criterion
Here is an analysis of each new criterion, the “critical elements” that comprise the criterion, and the ACCME’s standard for compliance, with additional interpretation and analysis.
Bucket 1—Inclusive Teaching and Learning
Criterion 23—Engages in Interprofessional Collaborative Practice in the Planning and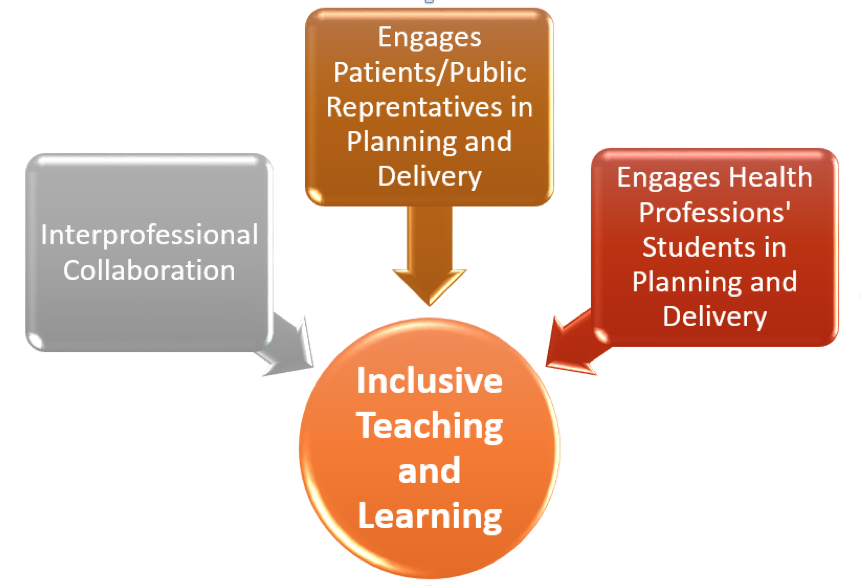 Delivery of Interprofessional CE (IPCE)
Delivery of Interprofessional CE (IPCE)
Rationale—Interprofessional collaborative practice can be defined as where multiple health workers from different professional backgrounds work together with patients, families, caregivers, and communities to deliver the highest quality of care. IPCE is demonstrated when members from two or more professions learn with, from, and about each other to enable effective collaboration and improve health outcomes. This criterion will reward accredited providers that work collaboratively with multiple health professions to develop interprofessional continuing education.
Markers of Compliance
- Frequency: Greater than 25 percent of activities and/or learners.
- Substantive Manifestation: (a) Documentation that selected activities included planners from more than one profession who are representative of the target audience, AND (b) documentation that selected activities include faculty from more than one profession representing the target audience, AND (c) educational outcomes evaluate impact on the team.
Interpretation and Analysis
We suspect that additional PARS fields will include check boxes for each new criterion, which when checked will determine the frequency. Substantive documentation will in all likelihood be demonstrated in the self-study chapter narrative and in attachments to that chapter using two to four explicit examples showing the above three manifestations.
Criterion 24—Engages Patient/Public Representatives in the Planning and Delivery of CME
Rationale— Accredited education needs to advance the interests of the people who are served by the healthcare system. It is important to involve patients and the public in the planning and delivery of CME. This criterion rewards providers that incorporate patient and public representatives as planners, teachers, and learners in the accredited program. Listen to the SP&A interview with Dr. Sandeep Pulim from @ Point of Care by clicking on this link.
Markers of Compliance
- Frequency: Greater than 25 percent of activities and/or learners.
- Substantive Manifestation: (a) Documentation that selected activities included patients and/or public representatives who are not healthcare professionals, AND (b) documentation that selected activities include teachers who are patients and/or public representatives who are not healthcare professionals.
Interpretation and Analysis
In addition to new PARS checkboxes for each new criterion, documentation will in all likelihood be demonstrated in the self-study chapter narrative and in attachments to that chapter using two-to-four concrete examples showing the above two manifestations.
Criterion 25—Engages Health Professions’ Students in the Planning and Delivery of CME
Rationale— CME is an integral part of the continuum of medical education and needs to continually evolve to support emerging generations of health professionals. Student engagement in planning and delivering activities will facilitate the development of CME that will meet their needs as future participants. This criterion rewards providers for building bridges across the education continuum and for creating an environment that encourages students and professionals to work together to fulfill their commitment to lifelong learning.
Markers of Compliance
- Frequency: Greater than 25 percent of activities and/or learners.
- Substantive Manifestation: (a) Documentation that selected activities included planners that are health professions’ students, AND (b) documentation that selected activities include teachers who are health professions’ students.
Interpretation and Analysis
In addition to the new PARS checkboxes for each new criterion, documentation will in all likelihood be demonstrated in the self-study chapter narrative and in attachments to that chapter using two to four concrete examples showing the above two manifestations. Listen to the SP&A interview with Leslie Lynch from OhioHealth on the integration of health professions’ students into CME planning by clicking on this link.
Bucket 2—Addressing Public Health Priorities
Criterion 26—Provides CME about Health Informatics and the Use of Practice Data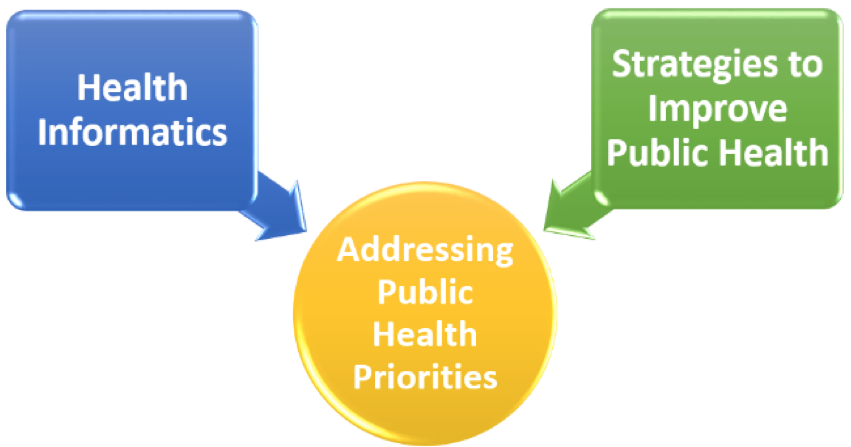
Rationale— The collection, analysis, and synthesis of information derived from the care of patients (i.e., health information) and the application of the lessons learned from these data contribute to healthcare improvement. This criterion will reward providers that teach about health informatics and teach learners how to apply the wisdom gained from practice data for practice and/or quality improvement.
Markers of Compliance
- Frequency: Greater than 10 percent of activities.
- Substantive Manifestation: Documentation that selected activities included content that documents development and implementation of CME on health informatics or the use of practice data
Interpretation and Analysis
In addition to new PARS checkboxes for each new criterion, documentation will in all likelihood be demonstrated in the self-study chapter narrative and in attachments to that chapter using two to four examples. Health informatics can be a standalone activity or included in other clinical activities. This is critical knowledge that physicians need to have today to manage their practice and should be included in all curricula. Key competencies that can be taught include:
- Find, search, and apply knowledge-based information to patient care and other clinical tasks
- Effectively read and write from the electronic health record for patient care and other clinical activities
- Use and guide implementation of clinical decision support
- Provide care using population health management approaches
- Protect patient privacy and security
- Use information technology to improve patient safety
Listen to the SP&A interview with Dr. William Hersh from Oregon Health & Sciences University on informatics by clicking on this link.
Criterion 27—Provides CME about Implementation Strategies to Improve Public Health
Rationale—This criterion rewards providers for expanding their programs beyond clinical care education to address factors affecting the health of populations. To achieve compliance, the accredited program will teach learners how they can implement change in health behaviors, social and economic factors, and the public’s physical environment.
Markers of Compliance
- Frequency: Greater than 10 percent of activities.
- Substantive Manifestation: (a) Documentation that selected activities included content that documents development and implementation of CME that directly addresses public health concerns, AND (b) content that includes strategies to achieve improvements in public health.
Interpretation and Analysis
In addition to new PARS checkboxes for each new criterion, documentation will in all likelihood be demonstrated in the self-study chapter narrative and in attachments to that chapter using two-to-four concrete examples. Content that addresses the Health of Populations can and should be included as an integral part of clinical education, especially where clinical change and improvement alone is not sufficient to resolve the public health issue. Factors that affect the Health of Populations are demonstrated in the chart below:
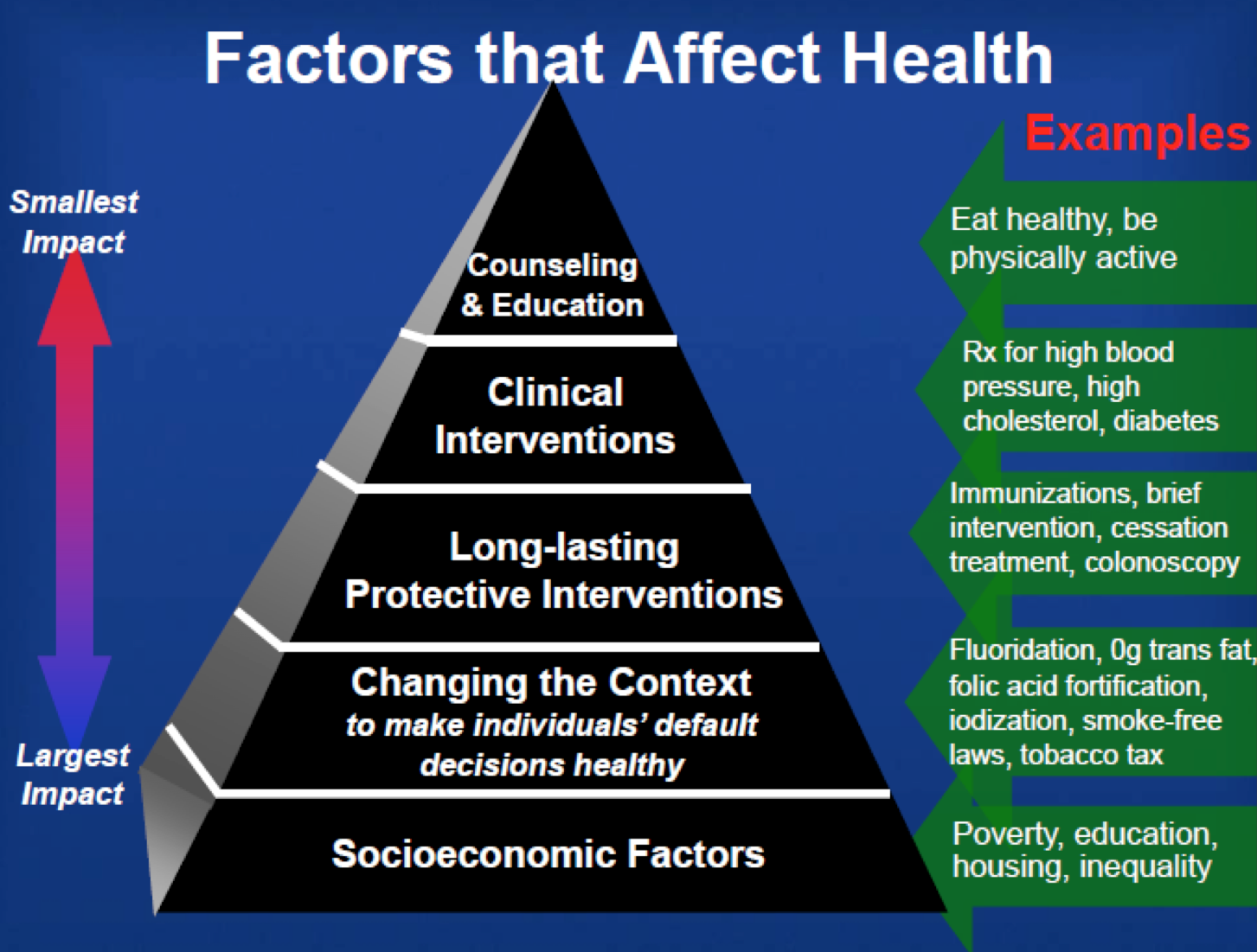
Listen to the SP&A interview with Dr. Julie Willems Van Dijk on factors affecting the health of populations by clicking on this link.
Bucket 3—Creating Behavioral Change
Criterion 28—Develops Communication Skills of Learners
Rationale—Communication skills are essential to most aspects of professional practice.  This criterion will reward providers that help learners become more self-aware of their communication skills, and implement educational interventions to improve those skills.
This criterion will reward providers that help learners become more self-aware of their communication skills, and implement educational interventions to improve those skills.
Markers of Compliance
- Frequency: Greater than 10 percent of learners and/or activities.
- Substantive Manifestation: (a) Documentation that selected activities included and objective assessment of communication skill, AND (b) provides feedback to the clinical-learner using the assessment.
Interpretation and Analysis
In addition to new PARS checkboxes for each new criterion, documentation will in all likelihood be demonstrated in the self-study chapter narrative and in attachments to that chapter using two to four concrete examples. Communication skills training can be added onto many clinical education activities as a mechanism to overcome communication barriers that can undermine the achievement of intended results. The requirement for individualized assessment and feedback can be daunting, but technology can assist in this process.
Criterion 29—Develops Technical and Procedural Skills of Learners
Rationale—Technical and procedural skills are essential to many aspects of professional practice, and can need updating, reinforcement, and reassessment. This criterion will reward providers that help learners gain technical and procedural skills.
Markers of Compliance
- Frequency: Greater than 10 percent of learners and/or activities.
- Substantive Manifestation: (a) Documentation that selected activities included and objective assessment of technical or procedural skills, AND (b) provides feedback to the clinical-learner using the assessment.
Interpretation and Analysis
In addition to new PARS checkboxes for each new criterion, documentation will in all likelihood be demonstrated in the self-study chapter narrative and in attachments to that chapter using two-to-four concrete examples. Technical and procedural skills training can be standalone education in workshops, labs, and sim centers, or added onto didactic modules. Skills trainings can be formalized as per AMA PRA skills training special credits with proctors, or less-formalized processes. The requirement for individualized assessment and feedback can be daunting, but technology can assist in this process. Listen to the SP&A interview with Beverly Hughes and Dr. Michael Brannick from the University of South Florida on proctor-ready skills education by clicking on this link.
Criterion 30—Creates Individualized Learning Plans for Learners
Rationale—This criterion rewards providers for developing CME that is designed to address the specific needs of an individual with a customized set of educational interventions. The baseline individual practice gap may be derived from a variety of sources. The provider creates an individual, longitudinal curriculum for each learner, or customizes an existing curriculum for the learner. The personalized education needs to be designed to close the individual’s professional practice gaps. Providers are expected to repeatedly evaluate and provide feedback to the learner about their competence, performance, or patient outcomes relative to the identified gaps and needs.
Markers of Compliance
- Frequency: Greater than 10 percent of learners and/or activities.
- Substantive Manifestation: (a) Repeated assessment of the individualized learner, AND (b) provides feedback to the individual learner, AND (c) provides individualized recommendations to learners of activities that close learning gaps.
Interpretation and Analysis
In addition to new PARS checkboxes for each new criterion, documentation will in all likelihood be demonstrated in the self-study chapter narrative and in attachments to that chapter using two to four concrete examples showing the above three manifestations. Individualized learning plans, education, and assessment will not be for every CME provider. Providers that embark on this type of education will need to identify a course champion who can identify appropriate learners, counsel and coach learners, assist with the development of learning plans for each learner, and follow through with assessment and feedback.
Criterion 31—Provides Services and Resources to Generate and Sustain Long-Term Behavioral Modification of Learners
Rationale—Repeated engagement can sustain change. This criterion will reward providers that create supplemental services (e.g., reminders) and resources (e.g., instructional material online) that have meaningful ongoing utility to learners. The provider can demonstrate that their resources have value by tracking and reporting utilization.
Markers of Compliance
- Frequency: Greater than 10 percent of learners and/or activities.
- Substantive Manifestation: (a) Use of ancillary tools and resources (e.g., reminders, repeat assessments similar to old Criterion 17, AND (b) demonstration that the ongoing use of the system or resources provided to learners have produced value.
Interpretation and Analysis
In addition to new PARS checkboxes for each new criterion, documentation will in all likelihood be demonstrated in the self-study chapter narrative and in attachments to that chapter using two to four concrete examples showing the above two manifestations. This criterion no longer stops at the offering of ancillary tools and resources, but will require modification of performance outcomes measurements to track use of tools and resources to demonstrate value.
Bucket 4—Demonstrating Leadership
Criterion 32—Engages in CME Research and Scholarship
Rationale—CME professionals should share best practices by developing and supporting  innovative approaches, studying them, and disseminating the findings with our healthcare education community. This criterion is designed to encourage and reward this scholarly effort.
innovative approaches, studying them, and disseminating the findings with our healthcare education community. This criterion is designed to encourage and reward this scholarly effort.
Markers of Compliance
- Frequency: Once every year of the Accreditation Cycle.
- Substantive Manifestation: (a) Conducts research relevant to CME, AND (b) produces data or information relevant to CME, AND (c) publishes abstract or manuscript in a peer-reviewed journal.
Interpretation and Analysis
This criterion will be applicable to providers that publish their work and innovations in the CME literature or other peer-reviewed publications. It will require either four or six such studies and publications to demonstrate compliance for this criterion, depending on the number of years of the provider’s accreditation. Because of the requirement for the work to be published in a peer-reviewed journal and for the number of times such studies and publications are required, many providers will not find this criterion of interest. Listen to the SP&A interview with Dr. Curt Olson from the Geisel School of Medicine on research and scholarship by clicking on this link.
Criterion 33—Engages in Continuous Professional Development as Educators
Rationale—CME professionals need to maintain and develop their own skills. This criterion will reward providers if the majority of the CME team has participated in continuing professional development (CPD) in domains relevant to the CME enterprise.
Markers of Compliance
- Frequency: Greater than 50 percent of the CME team must participate in external CPD activities annually.
- Substantive Manifestation: Participation in the annual or regional Alliance for CEHP meetings, participation in ACCME workshops, participation in other seminars, webinars, or events that further educational skills and competencies.
Interpretation and Analysis
This criterion should be achievable for most CME providers. 50 percent of the CME team must participate annually in CPD activities. Providers should chart CPD training that each member of the team attends to qualify. This is an area about which you may wish to ask the ACCME to clarify of the meaning of “external activities,” since many providers conduct internal educational workshops on meaningful educational topics that are as effective as “external” activities. Listen to the SP&A interview with Steve Weinman, RN, from the Institute for Medical and Nursing Education, on CPD for the CME team by clicking on this link.
Criterion 34—Creates Collaborations with Other Organizations to More Fully Achieve Healthcare Goals
Rationale—A system in which organizations and people cooperate or collaborate with each other is a stronger, more empowered enterprise. This criterion will reward providers that apply this principle by creating collaborations that enhance the efficacy of the education.
Markers of Compliance
- Frequency: Greater than 10 percent of activities.
- Substantive Manifestation: (a) Demonstrates that the provider engages with other healthcare or community organizations, AND (b) collaborates within the initiative with others to improve healthcare, AND (c) generates meaningful and measurable collaboration.
Interpretation and Analysis
This criterion is similar to old Criterion 20. While those providers that were compliant with old C20 should have been documenting the three critical elements above, now at least 10 percent of all activities certified for CME must document the names of community or healthcare organizations with whom they collaborated, ensure that the collaboration is related to a meaningful improvement in the improvement in healthcare, and that the results of the collaboration are assessed.
Criterion 35—Demonstrates Creativity or Innovation in the Development or Delivery of CME
Rationale—Education is evolving and CME programs should demonstrate leadership and creativity by designing and implementing innovative programs that improve the efficiency, efficacy, and impact of CME on learners, systems, patients, and our communities.
Markers of Compliance
- Frequency: Once for every year of the Accreditation Cycle.
- Substantive Manifestation: The provider must demonstrate the use of an educational approach that was novel, creative, or innovative in the field of CME at the time it was launched.
Interpretation and Analysis
For providers that innovate new technologies and learning processes in CME, this criterion will be a way to show the work you do. However, this criterion is looking for truly novel approaches and either four or six of them will need to be demonstrated, depending of the length of the provider’s accreditation cycle. Listen to the SP&A interview with Dr. Sandeep Pulim from @ Point of Care by clicking on this link.
Bucket 5—Achieving Outcomes
Criterion 36—Demonstrates the Impact of the CME Program on the Performance of Individual Health Professionals
Rationale—This criterion takes accredited CME beyond designing activities to change  performance and measuring whether change occurred. This criterion will reward providers that can demonstrate the impact on the performance of individual learners.
performance and measuring whether change occurred. This criterion will reward providers that can demonstrate the impact on the performance of individual learners.
Markers of Compliance
- Frequency: Demonstrated impact on performance for greater than 10 percent of the program’s learners, OR measured impact on performance for greater than 25 percent of the program’s learners.
- Substantive Manifestation: (a) Measures performance of individual health professionals, AND (b) demonstrates the impact on the performance of individual health professionals, AND (c) connects the impact of performance to the learning activity(ies).
Interpretation and Analysis
With an emphasis on measurement of true performance outcomes, this criterion connects easily with new Criterion 30 (individualized learning plans), but it may also link to any other activities in which the provider is able to engage with the learner in individualized outcomes measurement related to performance. This criterion can be achieved with the use of one-on-one interviews of either 10 percent or 25 percent of learners depending which value will be used in demonstrating compliance with the Criterion. The use of new technology that allows individual learners to demonstrate performance outcomes that are specific and quantifiable will be useful for larger audiences of learners.
Criterion 37—Demonstrates the Impact of the CME Program on Process Improvement
Rationale—Changing processes of care is often a key step that enables improvements in patient outcomes and safety. This criterion rewards providers that can demonstrate the impact of the CME program on process and/or quality improvement.
Markers of Compliance
- Frequency: Demonstrated impact on process(es) or quality of care for greater than 10 percent of program’s learners, OR measured impact on process(es) or quality of care for greater than 25 percent of program’s learners.
- Substantive Manifestation: (a) Measures processes of care, AND (b) demonstrates the impact on the process and/or quality improvement, AND (c) connects the impact on process and/or quality improvement to the learning activity(ies).
Interpretation and Analysis
This Criterion will apply in general to health care institutions and systems in which the CME program has been linked effectively to quality improvement and there is an ongoing relationship with the QI department at the institution or system. It would also apply to any CME provider that has established a collaborative relationship with the point of care so that quality improvements can be quantified and measured. Listen to the SP&A interview with interview with Mary Strong and Dr. Mark Jarrett from Northwell Healthcare by clicking on this link.
Criterion 38—Demonstrates the Impact of the CME Program on the Health of Patients/Communities
Rationale—Our shared goal is to improve the health of our patients and communities. This criterion rewards providers who can demonstrate the impact of the CME program on improvements in the health of patients/communities.
Markers of Compliance
- Frequency: Demonstrated impact on the health of patients/communities at least once in each year of the accreditation cycle, OR measured impact on the health of patients/communities at least once in each year of the accreditation cycle.
- Substantive Manifestation: (a) Measures patients / community health outcomes, AND (b) demonstrates the impact on the health of patients/communities, AND (c) connects the impact of the health of patients/communities to the learning activity(ies).
Interpretation and Analysis
Similar to Criterion 37, success with this criterion will fall to providers that can show that their CME program contributed to improvements in patient health in general and at the community level. Institutions with strong QI departments, and especially those with community health and population health units, will be successful. Listen to the SP&A interview with Mary Strong and Dr. Mark Jarrett from Northwell Healthcare by clicking on this link.
Steven Passin is the president & CEO of Steve Passin & Associates, based in Newtown Square, Penn. For questions, please contact Steve at [email protected].
NOTE: All interviews referenced were conducted in 2014 relative to the proposed commendation criteria. While the revised criteria are very similar, some criterion numbers may be different than those stated in the interviews.




